As a doctor, you are no stranger to the emotional intensity that comes with patient care. Whether it’s the distress of a new diagnosis, the frustration of chronic illness, or the anger of unmet expectations, you are often the first to witness and hold space for a patient’s emotional pain. While this deep empathy is a strength, it can also become overwhelming if you find yourself absorbing the emotions of your patients. Over time, this emotional burden can lead to exhaustion, burnout, and even a sense of helplessness.
So, how can you continue to provide compassionate care without being swept away by the emotional waves of your patients? Here are some practical strategies to maintain emotional boundaries while staying fully present and engaged in your work.
1. Empathy vs. Absorption: How to Set Emotional Boundaries as a Doctor
Empathy allows you to understand and connect with your patients’ emotions without becoming enmeshed in them. Absorption, on the other hand, occurs when you take on their emotions as if they were your own. Looking at the different components of empathy according to research1, Absorption reflects predominantly the element of Empathic Distress.
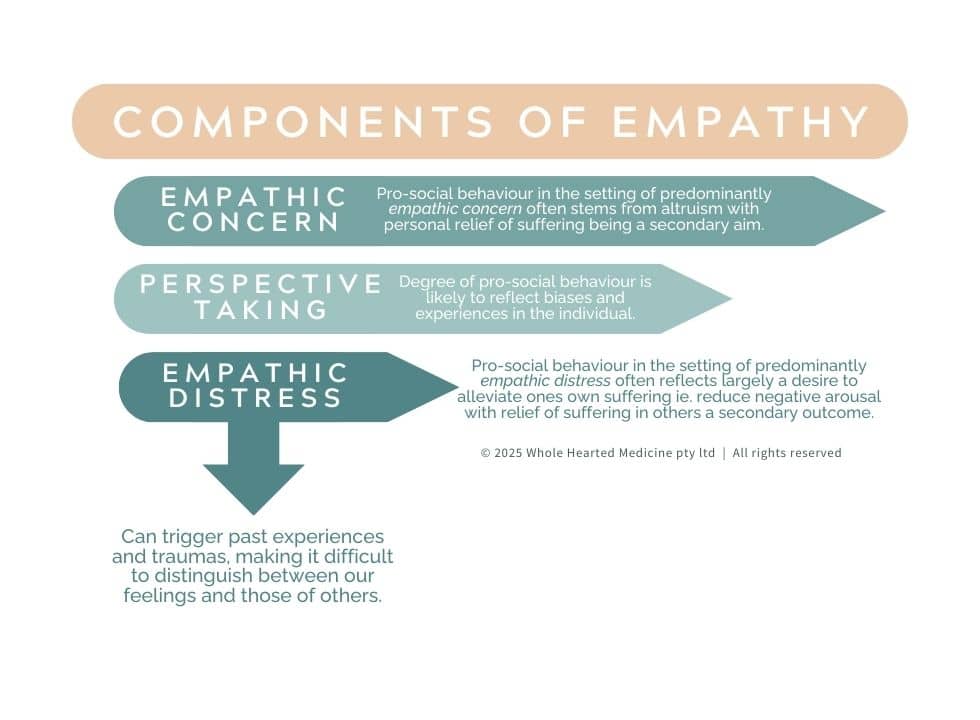
Patients will express their distress in many ways—anger, withdrawal, anxiety. It’s important to acknowledge their feelings without internalising them in order to remain connected to the more helpful components of empathy- Empathic Concern and Perspective Taking, without getting consumed by Empathic Distress. You might say to yourself, “This emotion belongs to them, not me” or visualise their emotion as a wave passing by rather than something you must absorb.
If you are finding it difficult to delineate between the patient’s emotions and your own, this is an important signal for you to consider what extra support you have in your life and move to access that. We all deserve an objective sounding board to tease out the tangled mess of emotions that can sometimes occur in the course of patient care.
2. Grounding Techniques for Doctors: Managing Emotional Overload
Developing a grounding ritual before and after emotionally intense patient interactions can help you maintain your emotional balance. This could include:
- A simple breathwork exercise—such as inhaling for four counts, holding for four, and exhaling for six—can help reset your nervous system.
- Setting an internal intention, such as “I can be present without taking this on as my own”, can also create an emotional boundary.
- Placing your feet firmly on the ground and feeling the support beneath you.
- Washing your hands after an appointment as a symbolic way to release any residual emotional weight.
- A short pause between consultations can make a big difference. Take a few deep breaths, stretch, or step outside for fresh air if possible. Even a moment to roll your shoulders and consciously release tension can help reset your emotional state.
These small yet intentional actions can serve as a reminder that while you are present for your patients, you do not need to carry their burdens with you.
3. Emotional Containment: Preventing Compassion Fatigue in Healthcare
Compassion and detachment may seem contradictory, but they can coexist. Compassionate detachment allows you to be deeply caring without becoming entangled in the emotional experience, Samuel Shem alludes to the importance of this skill of emotional containment in his book The House of God with the Third Law being “The patient is the one with the disease”. Think of it as being the steady lighthouse rather than the boat tossed in the storm. One way to practice this is to shift from feeling your patients’ emotions to witnessing them- you can acknowledge, validate, and support without carrying their burden as your own. Practicing the skill of mindfulness consistently (not just when you need it) can be an important part of being able to do this for yourself, especially when you need to call on it in stressful situations.
Visualisation techniques can also be a powerful way to create an internal boundary between yourself and your patients’ emotions. Some doctors find it helpful to:
- Imagine a protective barrier, such as a translucent shield or a boundary line, that allows compassion to flow freely while preventing emotional overwhelm.
- Visualise a river where emotions flow past without sticking, allowing you remain steady and present.
- Think of yourself as an air traffic controller, listening to your patient’s concerns with care and attention just as they would be watching the planes coming and going from the airport, without hopping on them.
Another technique is to picture placing the patient’s emotions in a mental container—acknowledging their pain but consciously deciding not to take it on as your own. This does not mean disengaging; rather, it is about holding space in a way that protects your own wellbeing.
4. Cultivate Self-Compassion
One of the reasons doctors may absorb their patients’ emotions is an internal belief that they must fix every problem or alleviate all suffering. While the desire to help is admirable, it is important to remind yourself that your role is to support, not to rescue.
Practicing self-compassion can help shift this mindset. Dr. Kristin Neff, a leading researcher in self-compassion, suggests using self-kindness instead of self-judgment, recognising our shared human experience, and staying mindful of our emotional state. When faced with a particularly difficult patient encounter, try offering yourself a moment of kindness: “This is hard, but I am doing my best” or “That was a difficult conversation. It makes sense that I feel this way”. This simple practice can help soften the emotional impact and reduce self-imposed pressure.
If you would like to try a free meditation designed to support healthcare professionals in practicing self compassion you will find one here.
5. Seek Support and Supervision
You do not have to process challenging emotions alone. Regular debriefing with trusted colleagues, mentors, or a professional supervisor can help you process difficult encounters in a healthy way. Sharing your experiences with those who understand can provide both emotional relief and valuable perspective.
If you find yourself consistently overwhelmed by patient emotions, consider seeking support from a professional who specialises in physician wellbeing. Therapy, coaching, or peer support groups can offer tools to strengthen emotional resilience and prevent burnout including some of the resources listed below:
- Drs4Drs– National network of Doctors Health Advisory services
- Balint Australia & New Zealand– Clinical reflective practice for doctors
- Capstan Partners– Coaching for Doctors & Health Professionals
- Doctors Who Coach Doctors– Network of independent doctor coaches
- The Black Dog Institute- The Essential Network for Health Professionals
- Mindcheck HP– Telehealth psychology for health professionals
6. Prioritise Your Own Wellbeing
Finally, your capacity to care for others is directly tied to how well you care for yourself. Make time for restorative activities that help you recharge—whether it’s exercise, time in nature, creative hobbies, or simply moments of stillness. Prioritising sleep, nutrition, and personal relationships also plays a crucial role in maintaining emotional resilience. No one single activity will stop you from feeling the stress of your work, but the more layers of self care and wellbeing that you put between you and your work will help to buffer difficult elements such as tough patient interactions and adverse outcomes.
This also includes holding the boundaries necessary to keep yourself well- such as professional boundaries around what you will and won’t do, physical boundaries around your personal space and time boundaries around what you say ‘yes’ and ‘no’ to- as uncomfortable as it can feel sometimes to enforce these, boundaries are an important aspect of your self care.

Remember: You are not just a doctor. You are a human being with your own emotional needs. By taking care of yourself, you not only protect your own wellbeing but also enhance your ability to provide sustainable, compassionate care.
Conclusion
Being present with your patients’ emotions without absorbing them is a skill that takes time and practice. By setting clear emotional boundaries, grounding yourself, practicing self-compassion, and seeking support, you can continue to provide exceptional care while safeguarding your own mental and emotional health. If you would like to explore ways to implement these skills and practices in your own life then don’t forget to check out our retreats and learning hub to find out how we can support you to do that.
Caring for others should not come at the expense of caring for yourself. By integrating these strategies into your practice, you can sustain your passion for medicine while maintaining your own sense of balance and wellbeing.
- Delgado N, Delgado J, Betancort M, Bonache H, Harris LT. What is the Link Between Different Components of Empathy and Burnout in Healthcare Professionals? A Systematic Review and Meta-Analysis. Psychol Res Behav Manag. 2023 Feb 15;16:447-463. doi: 10.2147/PRBM.S384247. PMID: 36814637; PMCID: PMC9939791.
↩︎


